Introduction
A supernumerary tooth is a number development aberration that is distinguished by the presence of a tooth in addition to the usual series.1 Its prevalence rate in the permanent dentition varies between 0.1% and 3.6% depending on the population, with a higher incidence in males than in women in a 2:1 ratio. 2 They can arise in practically any location of the dental arch, but have a significant propensity towards the premaxilla area (approximately 90%). They are found to be present in the maxillary arch more commonly than in the mandibular arch and although they can occur in both primary and permanent dentition, however their occurrence in primary dentition is very unusual. 2, 3
The cause of supernumerary teeth is not totally known. There are several hypotheses about the various sorts of supernumerary teeth. According to one view, the supernumerary tooth is formed as a result of a tooth bud dichotomy. (Liu, 1995) 4 The hyperactivity theory proposes that supernumerary teeth arise as a result of local, autonomous, conditioned hyperactivity of the dental lamina. Levine (1961). 5
Several studies have used cone beam computed tomography (CBCT) to accurately diagnose supernumerary teeth, overcoming most of the technical limitations of plain film projection and providing a high resolution three dimensional (3D) representation of the maxillofacial tissues. 1, 3 Treatment is determined by the type and position of the extra teeth, both clinically and radiographically. 2 CBCT pictures aid in precisely determining the form and precise location of the mesiodens.
The aim of this article is to describe rare cases of palatal placed, inverted, mesiodens that monitored at pediatric dentistry department while discussing the outcomes of using CBCT to diagnose the accurate position of supernumerary teeth and to choose the appropriate management technique.
Case Series
Case Report 1 (Under general anesthesia)
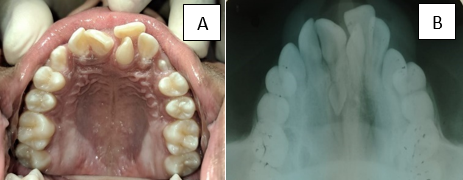
A 13-year-old male patient presented to the Department of Pedodontics with complaints of anterior tooth malalignment. There was a 2-year history of damage to the same tooth. Clinical examination reveals that there was a supernumerary teeth in relation to 21 (Figure 1A). An occlusal radiography examination revealed an inverted mesiodens adjacent to the root apex of the 11. (Figure 1B)
Figure 3
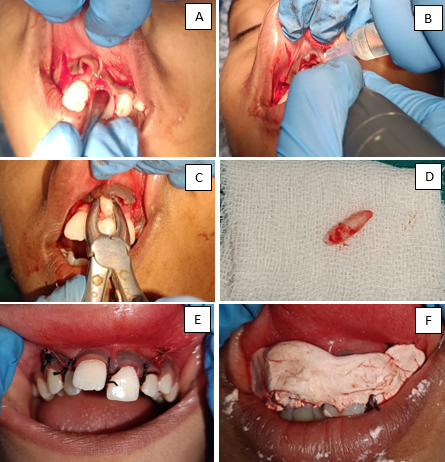
A: Palatal mucoperiosteal flap raise; B: Mesiodens extracted; C and 3D: Mesiodens; E: Suture given
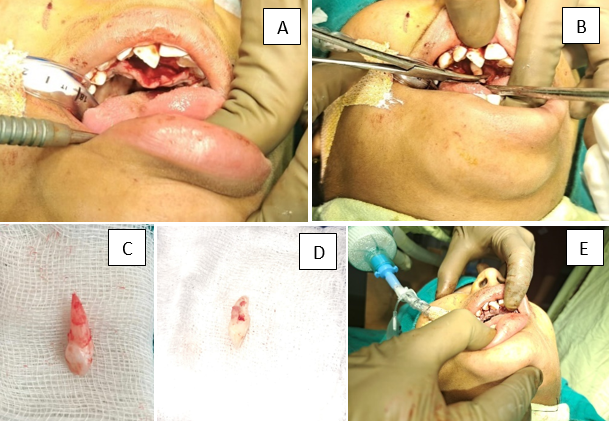
Figure 6
A: Palatal mucoperiosteal flap raise; B: Bone cutting; C and 6D: Mesiodens; E: Suture given; F: COE pack given)
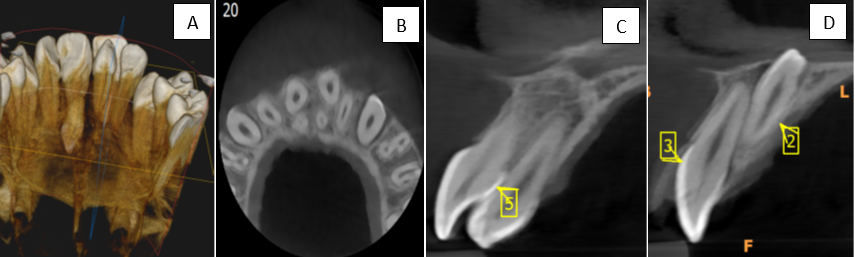
The patient was referred for CBCT of maxilla to assist the localization and orientation of the mesiodens. [Figure 2A] The CBCT showed that the presence of a two supernumerary tooth; moreover, the axial slice image of CBCT revealed the palatal position of the impacted and inverted mesiodens in relation to 11 and an erupted supernumerary tooth in relation to 21 [Figure 2B]. The sagittal slices showed that the supernumerary tooth was in palatal position over the root of permanent maxillary left central incisor [Figure 2C and D]. It classified as V3 (The mesiodens exists on the apical point to nasal floor)-H3 (Mesiodens distal to nasopalatine duct)-D2 (Inverted Mesiodens) according to kim et al. which is described in discussion section.
A comprehensive treatment plan was formulated, which included surgical extraction of the mesiodens and the supernumerary tooth under general anaesthesia (GA) because the tooth is in close relation to nasopalatine canal and perforating nasal floor. After obtaining pre-surgical assessment clearance the patient was admitted to the hospital. When GA is achieved, firstly erupted supernumerary teeth was extracted and after that, a full thickness palatal flap was raised using mucoperiosteal elevator. The mesiodens was exposed using bone cutting carbide bur, then luxated and removed. Haemostasis was achieved and mesiodens extracted socket packed with bone wax to prevent further bleeding and the flap was replaced back and sutured using 3-0 silk.
Postsurgical instructions were explained to the patient. Antibiotics and analgesic were prescribed to the patients. After 7 days patient was recalled to remove suture and to evaluate the healing process.
Case Report 2 (Under local anesthesia)
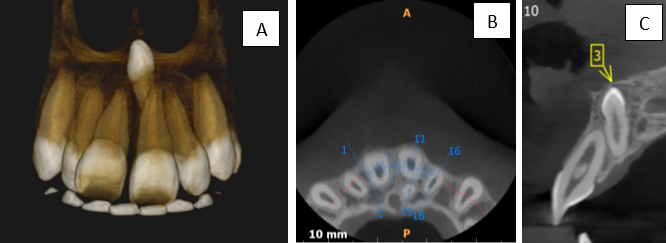
A 12-year-old male patient reported to the Department of Pedodontics, complaining of malalignment of teeth in upper front region. Aesthetic was the only primary concern of the patient. There was no relevant medical and family history, and the patient was otherwise healthy with no associated syndrome. On clinical examination, the patient was found to be in a permanent dentition stage and in addition, 11 overjet relation to lower anteriors. (Figure 4) No interference with the occlusion was noted, and the soft-tissue appeared normal. To investigate further CBCT was carried out to evaluate the status of the mesiodens, as well as the other teeth. Blood investigations were done and the reports were within normal limits. Here Mesiodens in classified as V2 (The mesiodens exists middle of the root to apical point)- H1 (Mesiodens lies in dental arch to labial side)- D2 (Inverted mesiodens).
The pathology was detected on CBCT. It is found that there inverted conical mesiodens present palatal to 21 and crown of mesiodens tilted with the roots of 11 resulting in proclination of the 11. (Figure 5) Treatment plan surgical extraction of mesiodens under local anesthesia (LA). Infraorbital and nasopalatine block was given using lignocaine 2% epinephrine 1:100.000). As the mesiodens crown was placed buccally and root in palatally. So buccal flap was raised for mesiodens removal.
From #23 to #13, a complete mucoperiosteal vestibular incision was done just above the mucogingival junction (1-2 millimetres superior). To disclose the impacted supernumerary teeth, subperiosteal dissection of the labial mucosa was undertaken. Under saline irrigation, bone above the mesiodens was removed using a bone cutting bur, and the crown of the mesiodens was revealed (Figure 3), before the mesiodens was luxated and removed. The sockets and incision region were washed with saline after the mesiodens were elevated and extracted. After that, the exposure was closed with 3-0 silk suture and covered with COE- pack. Anti-inflammatories and antibiotics were prescribed to the patient. The patient had no post-operative problems. Seven days later, the sutures were removed.
Discussion
Morphologically, the mesiodens is a primitive tooth with a cone form and a lesser size than regular teeth. It may show with a tuberculate form or imitate a genuine tooth at times. The root is usually completely developed and globular in shape. The mesiodens is most commonly located on the palatal side, between the upper central incisors, along the sagittal median plane.6, 7 All mesiodens have a conical crown and a short conical root.8
Kimura et al (2023) 9 summarized the categorization for the position and direction of mesiodens determined using CBCT and exhibited the variations found in the surrounding bone thickness. Distinct forms of mesiodens impactions and orientations necessitate distinct surgical methods and access. The categorization of mesiodens, as well as the link between the surgical method and the affected location, remain unknown. Using the anatomical structure as a guide, we grouped the mesiodens into three groups (V, vertical position; H, horizontal position; and D, direction of impaction) and classified them into three degrees for each group.
Vertical position classification
In the sagittal plane of the CT, the vertical locations of the mesiodens were divided into three degrees using the central incisors as a reference [Fig. 7]. V1-the mesiodens exists on the crown side from the center of the central incisor root to the apical point, V2-the apical point to the nasal floor, and V3-the apical point to the nasal floor. The central incisors were utilized as a reference by Kim et al. and Cheong et al. to classify the vertical placements.10, 11 The central incisors and nasal floor were utilized as references by Goskel et al.12 By dividing the bone region from the nasal floor to the alveolar bone ridge, Sano et al. divided the vertical position into three degrees. 13
Horizontal position classification
In the axial plane, we identified the horizontal positions where the mesiodens were placed [Fig 7]. H1 indicates the area between the dental arch and the labial side, H2 represents the area between the palatal side of the dental arch and the nasopalatine duct, and H3 represents the distal area of the nasopalatine duct. 10
Classification of impaction direction
We divided impaction direction into three degrees using sagittal, axial, and coronal planes: D1-normal, D2-inverted, and D3-horizontal. The location of the mesiodens and the alveolar bone are measured. M: the position on the mesiodens where the bone thickness between the mesiodens and the palatal surface is the thinnest. P: the location on the palatal surface where the bone thickness between the mesiodens and the palatal surface is the thinnest. N: the nasal plane point at where the vertical line from P to the nasal plane connects. I: The point on the maxillary central incisor root at where the vertical line from M-P to M contacts the maxillary central incisor. [Fig.7]
The nasal floor approach may be thought of as the H1 and H2 mesiodens, where the angle between the nasal floor line and the axis of the mesiodens is less than 90 degrees. In contrast, in H3, the palatal approach is sometimes easier to remove than the nasal floor approach, even though it erupted from the nasal floor. Mesiodens on the high and far sides (V3 and H3) were extracted more frequently under general anesthesia, as we did in our instance. We think that the amount of bone removed is connected to surgical invasion, and that the choice of general anesthetic may be affected by this. Aside from bone removal, one of the elements influencing surgical invasion is the range of the mucoperiosteal flap to access the bone surface. Traditional extraction of deeply impacted inverted mesiodens with palatal position relative to the roots of the central incisors requires excessive bone removal and is associated with a high risk of injury to adjacent structures such as permanent teeth or their blood supply. As a result, most practitioners choose general anaesthetic or profound sedation, which need hospitalization and anesthetic drug administration. Another critical element is to undertake the surgical intervention before the onset of dental developmental disorders or malocclusion. The inverted mesiodens with perforating nasal floor in Case 1 is remarkable. The tooth was unusually placed, with the crown pointing anterior and the root facing posterior. The mesiodens found in the nasal cavity may develop into cystic forms or erupt. Despite all of the problems associated with mesiodens, extraction was carried out. Because the mesiodens is inverted and perforating the nasal floor, we performed case 1 under general anesthesia to provide a painless surgery and patient comfort. Furthermore, their involvement in the nasopalatine canal may produce in discomfort during LA administration. Other issues observed in the use of traditional surgical techniques include nasal mucosal perforation, more difficult extraction due to crown orientation, a lack of a solid grip for the elevator or forceps, and limited sight. Additionally, severe sedation may cause sobbing, vomiting, intravenous site discomfort, and aspiration. Because of the variable orientation of the mesiodens, the crown section of the mesiodens is positioned buccally and the root is located palatally in instance 2. So, in example 2, the intraoral vestibular technique gives much greater vision and has less problems in terms of traumatization of the neighbouring tissues. The most important issue here is detailed with a thorough evaluation of the position of the mesiodens, which leads to careful planning of the surgical approach and estimation of the required amount of nasal floor deflection and the level of discomfort it may cause during local anaesthesia, which was made perfectly clear before surgery in our study using CBCT.
Conclusion
The categorization for the location and direction of mesiodens using CBCT information, as well as the link between the positions of the mesiodens and the surgical strategy for removing them, were reported in this case report with evaluation of literature. It was discovered that the bone thickness around the mesiodens, surgical approach, and choice of anesthetic method differed depending on the position of the mesiodens. Most extractions were done utilizing the labial method for mesiodens on the labial side and the palatal technique for mesiodens on the palatal side. However, because of the near closeness to the nasopalatine duct, the palatal floor technique was adopted in case 1 mesiodens was positioned in V3 position. Because the palatal bone thickness in V3-H2 was larger than that in V3-H3, the nasal floor approach was employed more frequently, particularly in V3-H2-D2. In other words, owing of the reduced bone thickness around mesiodens in the palatal distant area, the palatal technique was used to remove them even at higher locations. So, we need proper radiographic examination for proper approach and anesthesia required for the extraction of mesiodens.