Introduction
In orthodontics it is difficult to determine the exact amount of time for correction of various malocclusion. In todays world every individual is preoccupied with work and looks for treatment alternatives which would save time irrespective of the cost involved.
Long orthodontic treatment also demands patience and maintenance of good oral hygiene for prolonged period of time. In case of poor oral hygiene dental caries, gingivitis and tooth mobility may become an issue. Prolonged forces on teeth may also lead to root resorption which will be detrimental for the patient in the long run.
Advances in orthodontics procedures are reported every now and then. There are certain treatment modalities which are already established and are being practised by the specialist which help in delivering the desired result within stipulated time. Some of the techniques involved are
Discussion
Before proceeding towards different techniques and procedures related to accelerated orthodontics, different phases of tooth movement must be understood.
There are three phases of tooth movement: 1
The Initial Phase: The initial phase of tooth movement involves rapid tooth movement due to its displacement in PDL space. It lasts for 24 hours to 2 days.
The Lag Phase: This phase shows no tooth movement because the hyalinised tissue formed in the PDL space on the compressed side due to orthodontic forces makes tooth movement difficult. By the process of undermined absorption the hyalinised tissue is removed in due course of time. It lasts from 4-20 days.
The Postlag Phase: In this phase the compressed side of PDL exhibits frontal resorption and bone remodelling which occurs at a constant rate which helps the tooth to move. This process starts after 40 days.
Table 1
Different methods of accelerating tooth movement are:
Surgical method
Corticotomy2
Corticotomy is a surgical technique by which cortical bone is cut but the underlying spongiosa is left intact. Cortical bone is hard and resistant in nature and offers maximum resistance to tooth movement. Once its cut the resistance to tooth movement reduces. The underlying spongiosa provides nutrition to the overlying cortical bone. Corticotomy can be done when single or multiple tooth movement is required. The cortical bone is cut both bucally/ labially as well as lingually in the entire alveolar height. Bone is also cut above the apices of teeth horizontally (Figure 1).
Corticision3
In this technique, after local anaesthesia administration, a reinforced surgical blade (No. 15T) is used. The blade is capable of making a surgical incision of 400
Piezocision4
One week after the placement of fixed orthodontic appliance, an incision is made in the buccal interproximal region through which a piezotome tip is inserted and 3mm deep piezoelectrical corticotomy is done. This results in temporary demineralization of the localized area where the surgery has been performed followed by increased remineralization. As compared to bur corticotomy effect of regional acceleratory phenomenon lasts for about 6 months (Figure3).
Advantages
Used in cases where movement of teeth is required in both arches at the same time.
Used in cases when localized tooth movement is required in a particular arch.
Used in cases where tooth movement is required at different times during treatment to achieve specific result.
Good periodontal tissue response.
Excellent aesthetic outcome.
Piezopuncture5
It is a technique in which a piezotome is used to create multiple punctures in the cortical bone through the overlying gingival. It works on the principal that when voltage is applied to polarized piezo ceramic, the piezo electric crystals gets deformed in the resultant electric field. This causes expansion and contraction of the material to which it is applied. It selectively cuts the mineralized tissue without damaging the adjacent soft tissue and nerves.
Micro-osteoperforation:6
Micro-osteoperforation is a technique in which small size perforations are made in the bone around the tooth which accelerates the rate of tooth movement during orthodontic movement. Due to the procedure, cytokines are released which in turn recruit the osteoclasts to the site of injury and leads to bone remodelling.
Alveolar reshaping/ Periodontally Accelerated Osteogenic Orthodontics (PAOO): 7
In this technique the procedure is performed under intravenous sedation and local anaesthesia. Full thickness flap are raised on the buccal and lingual aspect of maxillary and mandibular teeth beyond the teeth apices. Vertical corticotomy cuts just short of the alveolar crests are made between the roots of the teeth and are extended beyond the teeth apices. Horizontal scalloped cortical cuts are also made. This design of selective decortications allows maximum medullary bone penetration. A resorbable material is placed over the decorticated area and flaps are sutured back in their place. Orthodontic treatment can be started 1 week before or 2 week after the surgery (Figure 4).
Advantages
It includes both advantages of corticotomy and alveolar surgery.
Reduction in the amount of dehiscence and fenestration.
Good visualization due to full thickness flap reflection.
Bone augmentation provides additional support to the roots of teeth and perioral musculature.
Decreased risk of apical root resorption.
Periodontal distraction
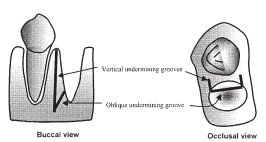
In this technique, after the extraction of tooth distal to the one which is to be retracted, distal inter-septal bone is undermined with a bone bur by grooving the bur vertically inside the extraction socket along with buccal and lingual sides. The depth of groove depends on the thickness of inter dental bone as determined by the peri-apical film.8 The bur is extended obliquely towards the base of interseptal bone so that the resistance to tooth movement can be weakened. The inter-septal bone is not cut mesiodistally. Following that a custom made intraoral distraction device is used on the buccal surface with an activation rate of 0.5-1 mm/day and power chain is used on the lingual side to prevent rotation of tooth (Figure 5).
Dentoalveolar distraction:9
In this technique, a horizontal incision is made parallel to gingival margin of canine and premolar beyond the vestibular depth. Holes are made in the cortex with the carbide bur 3-5 mm apically to root apex between canine and 2nd premolar which are then joined by tapered fissure bur. After the 1st premolar extraction its buccal bone is removed distal to canine and mesial to 2nd premolar. The alveolar segment around the canine is also mobilized. The palatal shelf is preserved but the apical bone near the sinus is removed leaving the sinus membrane intact.The dentoalveolar segment to be distracted includes the buccal cortex of canine and its underlying spongy bone leaving the palatal bone intact. Distraction is done after 3 days of surgery at the rate of 0.8 mm/day with the help of custom made distractor.
Mtdld technique: 10
Mtdld stands for monocortical tooth dislocation and ligament distraction. In this technique corticotomy is performed around each tooth which is to be moved. The buccal monocortical bone is cut and palatal ligament distraction is carried out simultaneously when applying biomechanical force. Buccal monocortical bone is cut laterally and apical to the tooth to be moved.
Mechanical / Device Assisted Methods
LIPUS (Low intensity pulsed ultrasound) 11
This technique uses ultrasound (mechanical energy) which is transmitted through different tissues as pressure waves. According to one study use of LIPUS at 0,3,5,7,14 and every 15 days increases the rate of tooth movement. The intensity of LIPUS application is 30-50Mu/cm2 for 15-20 min/day(Figure 6).
Resonance vibration
Nishimura et al.12 developed a vibration imposed system which applied forced vibration to teeth to measure its natural frequency. The vibrator was fixed to rat’s 1st molar with adhesive and vibrations were applied for 5 minutes at an acceleration of 1m/s2. A 0.012 NiTi expansive spring was fixed to 1st molar on right and left side for 21 days.12.8 g of force was applied to teeth and resonance frequency was loaded in a perpendicular direction on maxillary molar for 8 minutes once a week. Displacement was measured on 0,3,7,10,14,17 and 21 days after application of expansive force. The initial response of cells of cells appears within 30 minutes to mechanical stress (Figure 7).
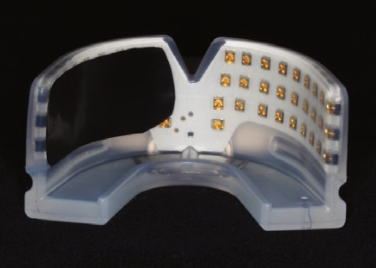
Photobiomodulation (Orthopulse LED Intraoral device) 13
Orthopulse is an intraoral appliance which is connected to a controller. The mouth piece has LED embedded in a tray like device made of silicone. Light is delivered through the buccal alveolar soft tissue into the alveolus. The device produces infra-redlight (850nm) peak wavelength. The patient receives 3.8 minutes of LED light/day per arch. The rate of tooth movement was 1.27mm/ week as compared to 0.44/week for control group (Figure 8).
Cyclic forces: 14
According to this method, cyclic forces when applied to teeth help in moving the teeth faster through accelerated bone remodelling. For this purpose a device called Accele Dent Type 1is used which consists of a removable device which is placed in patient’s mouth and other part is attached to it which is placed outside the mouth. The mechanical, electrical and energy components of the devie are housed in the extraoral device. The patient places the removable device inside the mouth once in a day for 20 minutes. A force of 0.2 N to 10 N is applied (Figure 9).
Direct electric current: 15
In this technique an electric device delivering a constant DC current of 15 microamperes is applied to the mesial and distal sides of the tooth to be moved. The tipping force on the canine produces compression on the distal aspect of canine and anode is placed on this side of the tooth. The electric cathode is placed near the tension side of tooth i.e. on the mesial aspect. Bone resorption is seen in area where anode is placed whereas bone apposition is seen in areas where cathode was placed.
Low intensity lazer therapy: 16
Mehta et al. carried out a split mouth experiment to evaluate the effect of low level lazer therapy on tooth movement. For this purpose, a lazer (800 nm) was placed on both buccal and lingual side of the canine to be retracted after 1st premolar extraction for a duration of 10 seconds. The canine was retracted using a closed NiTi coil spring with a force of 150g. On the control group no low level lazer therapy was used. The total energy density at each appointment was 8J. The canine on application of LLLT showed 29% increase in tooth movement in the maxillary and mandibular arches(Figure 10).
Magnets
Showkatbaksh et al.17 in a split mouth study on 10 patients showed the effect of pulsed electromagnetic field on tooth movement. A circuit and a watch battery were used to generate the pulsed electromagnetic field. The circuit was fitted to a removable device. The patient was instructed to wear the device which generated 1 Hz of electromagnetic field. The teeth on the control side were insulated from the effect of electromagnetic field with the help of a foil. The measurement on the control side and experiment side were made after 5 months and the diastema between the canine and 1st molar was measured to calculate the amount of tooth movement. The canine retraction on the magnetic field side was 1.57 mm more than the control group.
Chemicals/Pharmacological Approach
Parathyroid hormone
Soma et.al.18 conducted a study to evaluate the effect of Parathyroid Hormone on the orthodontic tooth movement.5 groups of 8 rats each were used. The first group was treated with vehicle infusion. The 2nd group was infused with PTH(1-84) 10μg/100g body weight/day. The third group was infused with 0.4 μg/100g bodyweight/day. The fourth group was infused with 4μg/100 body weight/day and the last group of rats was injected with 4μg/100g of body weight/day subcutaneously. After 24 hours of administration of PTH, movement of 1st molar was initiated by using closed coil spring which was ligated between incisors and 1st molars. A force of 30g for 12 days was used. The orthodontic tooth movement was evaluated by taking impression of maxillary cast at 3 day interval and measuring the diastema between 1st and 2nd molar respectively. The results showed that there was 50% increase in the distance between 1st molar and 2nd molar 3 fold increase in the osteoclast activity in group infused with 10μg/100g of bodyweight/day. On the 12th day of experiment the 1st molar movement in group 2 was twice as fast as in group 1. In the fifth group (PTH(1-34) injection) orthodontic tooth movement did not increased significantly. PTH(1-84) infusion did not affect the systemic bone metabolism whereas PTH(1-34) injection caused increase in bone mineral measurement and alkaline phosphatise.
Relaxin
Madan et al.19 conducted a study to evaluate the effect of relaxin on orthodontic tooth movement. The experiment group consisted of 120 rats. The maxillary incisors were stabalized by pinning them and mandibular incisors were reduced to prevent appliance damage. One end of closed NiTi coil spring was attached to the occlusal surface of the 1st molar and the other end was bonded to the maxillary incisors. Recombinant human relaxin was administered via minipump which was implanted subcutaneously slightly posterior to scapulae. Relaxin was delivered systematically via resorption through local capillaries at the rate of 5.3μg/hour/Kg. This resulted in blood concentration of 150 ng/ml. The results showed an increase in the rate of mobility of 1st molar upto 170% on day 1 and 130% on day 5 of relaxin administration.
Cytokine
Teixeira et al.20 conducted a study to measure the level of cytokines in PDL on orthodontic tooth movement. 48 rats were divided into 4 groups. To the 1st group a force of 50 Cn was applied to the maxillary 1st molar with the help of NiTi closed coil spring which was attached anteriorly to the incisors. In the 2nd group orthodontic force was applied to the 1st molar as well as flap was raised in the maxillary left molar region. In the 3rd group orthodontic force, flap and 3 shallow perforation of 0.25 mm depth were made. In the 4th group (control) no orthodontic force was applied. Bone labelling was done by intra-peritoneal injection of calcein (15mg/Kg) on day 0 and 26 and by demeclocycline (25mg/kg) on day 14. Expression of 92 different cytokines were studied after RT-PCR after 24 hours of force application. 37 cytokines were increased more than 2 fold in 1st, 2nd and 3rd group. Out of these 37, 21 cytokines /cytokine receptors were higher in orthodontic force, flap and perforation group.
Vitamin D3: 21
Ciur et al. conducted a study to evaluate the influence of local administration of Vit D3 on orthodontic tooth movement. Each arch is divided into 2 groups. One control and the other experimental quadrant. In the control quadrant the canine received conventional orthodontic treatment while the experimental quadrant received orthodontic therapy with intraligament injection od Vit D3. The experimental quadrant canine showed 70% greater increase in tooth movement as compared to control quadrant canine.
Platelet rich plasma: 22
Timamy et al. conducted a study on 15 female patients to check the efficacy of local injection of platelet rich plasma on the rate of orthodontic tooth movement. Split mouth study divided the mouth into 2 parts and canine retraction was done using 0.017 x 0.025 ss wire and NiTi closed coil spring. The intervention side was injected with 0.25 ml of platelet rich plasma in intraligament region in the middle, distobuccal and distopalatal areas of the distal surface of canines on day 0, 21 and 42 days. Results were evaluated using study model. Rate of tooth movement was 1.35 mm for control and 1.55 mm for experimental group.
Osteocalcin: 23
Hashimoto et al. conducted an experiment to study the effect of osteocalcin on orthodontic tooth movement in rats. 46 rats were divided into 6 groups of 6 rats each. The rats in the 3 experimental group were injected with purified rat osteocalcin at doses 0.1μg, 1μg and 10μg dissolved in 20 μl of phosphate buffered saline in the palatal subperiosteum adjacent to furcation of maxillary right 1st molar. The control group were injected with rat serum albumin. Elgiloy closed coil spring was ligated between incisors and 1st molar and the force of 30 g was used for protraction of 1st molar. The rats injected with1μg osteocalcin showed increase in tooth movement by 152%.
Thyroxine
Shirazi et al.24 conducted an experiment on rats to study the effect of thyroxine on orthodontic tooth movement. 50 male rats were used for the study and divided into 5 groups of 10 rats each. Orthodontic tooth movement was observed in 1 group without any intervention. In control group orthodontic appliance as well as 10ml/Kg intraperitoneal injection of normal saline was injected. In three groups, thyroxine was given at the rate of 5,10 and 20μg/Kg intraperitoneal /day along with the appliance. A 5 mm closed coil spring was used to protract maxillary 1st molar with a force of 60 g which was bonded anteriorly to incisors. The results showed that administration of intraperitoneal 20μg/Kg per day increased the amount of tooth movement.
Nicotine
Manal et al.25 conducted an experiment on 32 rats to see the effect of nicotine on orthodontic tooth movement. These rats were divided into 4 groups. Group A was injected with 0.37 mg/Kg nicotine ditartarate salt dissolved in normal saline solution. Group B received 0.57 mg/kg group received 0.93mg/kg nicotine.
Control group received a daily injection of 0.5 ml of normal saline for 28 days. Injection started 14 days before force application and orthodontic force and continued till the end of treatment. Group C showed the heighest rate of tooth movement (0.82 ± 0.063 mm) while control group showed the lowest mean score( 0. 23± 0.043 mm)
Prostaglandin
Leiker et al.26 conducted an experiment to study the effect of prostaglandins in rats. 112 animals were divided into 4 groups and were injected prostaglandin injections at the concentration of 0.1, 1.0, 5 and 10μg respectively. Half of the animals were injected with prostaglandins at the time of appliance delivery and the other half received weekly injections. A closed coil spring ligated between maxillary and incisors exerted a force of 60 grams. The conclusion drawn from the study was that a single injection of prostaglandin at a concentration of 0.1 and 1μg enhance orthodontic tooth movement.
Substance P
An et al.27 conducted a study to evaluate the effect of substance P on orthodontic tooth movement. 48 male rats were divided into 2 groups; The substance P group and control group. NiTi closed coil spring was fixed to the first molar and incisors and a force of 40 g was exerted. The rats in the substance P group received 5nmol/kg of intraveneous injections at 0, 24 and 48 hours after appliance delivery. The control group received 3 intravenous injections of buffered saline solution. On evaluation of tooth movement on day 7 and 14, the total tooth movement increased by 1.3 and 1.5 folds respectively.
Gene therapy
Kanzaki et al.28 in 2006 conducted an experiment to transfer the RANKL(Receptor activator of nuclear factor kappa-B ligand) gene locally to the periodontal tissue via a hemagglutinating virus of Japan(HVJ) envelope vector gene delivery system. The vector solution was administered in the palatogingival side of the maxillary first molar. A compressive spring was placed between the maxillary 1st molars causing them to move palatally. The distance between the gingival margins of the mid palatal cusps of the 1st molar before and after the orthodontic movement was measured with sliding callipers. Tooth movement on the RANKL transfection side was 0.63 ±0.06 mm as compared to control side (0.48± 0.05mm).
Conclusion
Time being a constraint in this progressive world forces us to find ways and means to complete a task in the most time efficient manner. Accelerated orthodontics is the result of this time management which deals with correction of crooked teeth in a manner different than the conventional style. Advantages of accelerated orthodontics is completion of treatment in minimum time possible for a particular case to provide a patient with functional and esthetic smile. However, accelerated orthodontics has some risks as well like root resorption and bone resorption particularly in invasive procedures. Adequate oral hygiene has to be maintained for achieving desired results within the stipulated time or else the treatment will get prolonged. Treatment with accelerated orthodontics depends on orthodontic problem, patient’s age, bone density, systematic disease and oral hygiene. Expertise on the part of orthodontist and oral surgeon are determining factor in achieving the desired result.