- Visibility 69 Views
- Downloads 40 Downloads
- DOI 10.18231/j.jds.2020.009
-
CrossMark
- Citation
Treatment of gingival recession on lower lateral incisor lingually using Mucograft® A Case Report
- Author Details:
-
Fariya Ashraf *
-
Sunaina Boro
-
Eiti Aggarwal
-
Rahul Chopra
-
Nikhil Sharma
Introduction
Gingival recession is the apical shift of the gingival margin with respect to the cemento-enamel junction (CEJ); which is associated with attachment loss and exposure of the root surface to the oral environment.[1] It causes dentinal hypersensitivity, unaesthetic appearance and if left untreated may lead to root caries, abrasion or cervical wear, erosion and an increase in accumulation of dental plaque.[2] There are various etiological factors which may contribute to gingival recession some of which may include various periodontal disease such as bone resorption, periodontal pockets, accumulation of plaque and calculus, mechanical forces such as improper flossing and tooth brushing, improper occlusal relationships, iatrogenic factors such as orthodontic tooth movements, anatomical factors including alveolar bone dehiscence, tooth mal-position,[3] aberrant frenal attachment as well as gingival morphology[4] and tongue piercings in case of lingual recession.[5]
Treatment of gingival recession on the lingual surface of mandibular anteriors is quite challenging, owing to difficulty in accessibility as well as anatomical constraints of this region. The goal of periodontal therapy is to regenerate the lost attachment of the tooth. Accordingly, it has become apparent over the past decade that a variety of regenerative procedures have the ability to correct gingival recession defects through augmentation of the height and width of keratinized gingiva, plus to gain partial or complete root coverage.
The widely used among these procedures include periodontal plastic surgical (mucogingival) graft techniques, either alone or in combination with guided tissue regenerative procedures.[6] Treatment of mandibular lingual recession is not a regularly performed treatment procedure due to its lack of esthetic significance, which is one of the most common suggestions for recession coverage.[7]
Sub-epithelial connective tissue graft (SCTG) is considered as a gold standard for treatment of recession defects, however it requires a donor site. Owing to this, there is always a quest for substitute techniques with lesser morbidity.
The “Tunnel” technique also known as “Supraperiosteal envelope” technique is a modification by Allen(1994) of Raetzke’s 1985 “envelope” technique. The tunnel technique has a minimally invasive nature since the interdental papillae are left intact and vertical incisions are not performed leading to better esthetic results.[8] This technique entailed the placement of a connective tissue graft in the tunnel. Bio-materials which can be used as a substitute in place of connective tissue grafts such as Mucograft®(Porcine) has gained importance recently due to its ease of application and no requirement of a previous preparation or hydration.[9]
Geistlich Mucograft® is a collagen matrix meant for recession defects and for the gain of keratinized tissue where open healing is required. It is stated to be designed to provide a requisite, reinforcing matrix and a signaling source for regenerative wound healing.[10], [11]
Case Report
A 28 year- old male patient reported to the Department of Periodontology and Oral Implantology, I.T.S. Centre for Dental Studies and Research, Murad Nagar with the chief complaint of dentinal hypersensitivity on the lingual side of the mandibular left lateral incisor. The patient described severe sensitivity to hot and cold liquids and a constant uneasiness in the mandibular lingual area. No relevant medical history was recorded and also there was no history of any type of habits.
Further, the periodontal evaluation revealed normal probing depths on the recessed tooth with mild plaque accumulation and minimal bleeding on probing. The patient presented with a narrow and deep gingival recession defect of 5mm and a lack of attachment on the lingual surface with respect to #32. No recession was there on the labial aspect of the same tooth. There was no mobility in any of the central and lateral incisors. The recession can be classified as Miller’s Class 2 on the facial with no interproximal bone loss and recession extending up to the mucogingival junction.[12] On radiographic examination, periapical radiographs revealed mild periodontal ligament space widening with mild to no horizontal bone loss interdentally.
After discussing the clinical findings, treatment options, and risks associated with the patient, oral and written consent was obtained for the same.
The treatment plan was divided in three phases: Presurgical phase which consisted of inflammation control through oral hygiene instructions, full-mouth debridement, and occlusal adjustment followed by Surgical phase which involved periodontal regenerative surgery of the area; and finally Maintenance phase, involving a strict supportive periodontal therapy (SPT).
Pre surgical phase
A full-mouth debridement along with slight occlusal adjustment were performed. Few necessary oral hygiene instructions were given and after re-evaluation the regenerative periodontal surgery was suggested.
Surgical phase
The patient was asked to rinse with 0.2% chlorhexidine digluconate solution prior to surgery. Local anesthesia of 2% lidocaine with 1/100,000 epinephrine was administered following which the exposed root surface was debrided with curettes.
Intrasulcular incisions were made on lingual surface of #31-33 with #15 blade. In order to undermine the lingual soft tissue, Orban’s knife (1/2 Allen Modified Orban Knife) was used. Further, Crescent Blade (CB01-2.5mm, 20 gauze) was used simultaneously in order to make the tunnel carefully and not to perforate it extending beyond the level of the mucogingival junction leaving interdental papillae intact. The mucoperiosteal tunnel was extended by full thickness preparation and laterally extended beyond the recession site up to #31-33 sites. All the attaching muscles and inserting collagen fibers were separated and released from the inner aspect of the tunneled flap in order to get the tension free flap which can be easily mobilized coronally. The interdental papillae were gently undermined to get complete mobilization of flap and thus a sub-periosteal tunnel or a pouch was created. Special care of interdental papillary tissues were taken and flap perforation was successfully avoided.
After tunnel preparation it was irrigated with saline and moist gauze was placed over it.
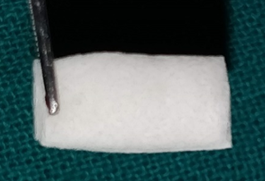
Further, a tin foil of appropriate size to be used in the receded area was measured and cut. Then the mucograft was cut according to the size of the tin foil. The Mucograft of appropriate size thus obtained was then moistened in saline solution and inserted within the prepared tunnel and stabilised using sling sutures.
Maintenance phase
The patient was prescribed 500 mg of amoxicillin TID for 7 days to prevent potential infection, 400 mg Ibuprofen BID for pain management and twice daily rinse with 0.12% Chlorohexidine rinse for 2 weeks. Patient was instructed to not brush the surgical area for at least 2 weeks. Sutures were removed at 2 weeks after surgery and returned to regular post-operative oral hygiene at 1 month and regular dental recall appointments.






Result
In the present case report, follow-up was done at 21 days which showed satisfactory root coverage as compared to the baseline. At baseline a gingival recession of 5 mm was recorded in the lingual aspect of mandibular incisor. After 21 days there was a reduction in gingival recession of up to 1.5mm. The surgical site was also completely healed. The patient expressed satisfaction as dental hypersensitivity was no longer reported.
Discussion
Gingival Recession is the apical migration of the gingival margin which leaves the root surface exposed to the oral environment leading to sensitivity, plaque deposition, caries etc along with unaesthetic appearance for the patient. Patients therefore often seek treatment for the gingival recession, which usually requires surgically covering the recession. Inflammation caused by calculus, prominent lingual freni, tongue piercings and deleterious habits are the most common etiological factors for lingual recession. But treatment for the same is not easy owing to the anatomical restraints which poses difficulty in any surgical procedure to be done, poor accessibility and difficulty in instrumentation of the area, tongue position, continuous salivary flow etc.
A case report by Vrushali et al., (2018)[13] in the treatment of Mandibular Anterior Lingual Recession Defect with Minimally Invasive Laterally Closed Tunneling Technique and Sub-Epithelial Connective Tissue Graft concluded that it is possible to successfully and predictably treat isolated lingual recession defects with a laterally closed tunneling technique and that the connective tissue graft still dominates effective method to cover exposed roots.
Moreira et al. (2013)[14] reported a clinical case using Mucograft® for root coverage with coronally positioned flap in a 4 mm recession Miller Class I. The results were satisfactory and, after 3 and 6 months of follow-up, the recession was completely covered. After 12 months, the gingival margin remained stable, and there was a maturation of the gingival tissue. According to the authors, the use of membrane for covering Miller Class I gingival recessions can be successful, but more randomized clinical trials demonstrating the predictability and efficiency of the material are necessary.
Another case report was done by Rotunda et al., (2012)[15] on the use of a new collagen matrix (Geistlich Mucograft®) for the treatment of multiple gingival recessions which showed three women with maxillary gingival recessions and were treated by means of the envelope flap technique associated with a novel collagen matrix as a substitute for the connective tissue graft. At 1 year, complete root coverage was achieved in 9 treated sites, with a mean keratinized tissue width of 3.1 mm, complete resolution of dental hypersensitivity, and a high level of esthetic satisfaction.
The SCTG which is considered a gold standard for treatment of gingival recession requires a donor site as well as long surgical procedure and patient discomfort. So in this present case report a minimally invasive tunneling technique along with Mucograft® has been presented that can restore the functional properties of lingual gingiva of the mandibular anterior teeth by repairing gingival defects and re-establish the integrity of the zone of keratinized gingiva.
Geistlich Mucograft® which is a porcine derived collagen matrix has shown optimal soft-tissue regeneration. It provides an alternative to autogenous soft-tissue grafts. Harvesting of the patient’s tissue is avoided, providing a benefit to both patients and clinicians.
However, a limitation of the graft is that it is not very economic and hence is not easily available.
There are very few case reports regarding the treatment of lingual recession and this case report is first of its kind to the author’s best of knowledge depicting use of Geistlich Mucograft® for lingual recession. However longer follow-up period is required to be more conclusive about the current technique used in this study.
Conclusion
It can be concluded that the Mucograft can be used as an alternative to sub epithelial connective tissue graft in the treatment of mandibular lingual recession with satisfactory result. However a longer follow up period is required to better assess the clinical outcome.
Source of Funding
None.
Conflict of Interest
None.
References
- A Mani, R James. Classifications for gingival recession: A mini review. Galore Int J Health Sci Res 2018. [Google Scholar]
- K Pradeep, P Rajababu, D Satyanarayana, V Sagar. Gingival Recession: Review and strategies in treatment of recession. Case Rep Dent 2012. [Google Scholar]
- WJ Gorman. Prevalence and etiology of gingival recession. J Periodontol 1967. [Google Scholar]
- S Ravipudi, D Apukuttan, P S G Prakash, Victor D J, G Recession. Short literature review on etiology, classifications and various treatment options. J Pharm Sci Res 2017. [Google Scholar]
- A Campbell, A Moore, EWilliams, J Stephens, D N Tatakis. Tongue piercing: Impact of time and barbell stem length on lingual gingival recession and tooth chipping. J Periodontol 2002. [Google Scholar]
- M M Kassab, R E Cohen. Treatment of gingival recession. J Am Dent Assoc 2002. [Google Scholar]
- G Assis, M Nevins, D Kim. The use of autogenous gingival graft for treatment of lingual recession on mandibular anterior teeth. Int J Periodontics Restor Dent 2017. [Google Scholar]
- A L Allen. Use of the supraperiosteal envelope in soft tissue grafting for root coverage. I. Rationale and technique. Int J Periodontics Restor Dent 1994. [Google Scholar]
- G N V Kumar, K R V Murthy. A comparative evaluation of subepithelial connective tissue graft (SCTG) versus platelet concentrate graft (PCG) in the treatment of gingival recession using coronally advanced flap technique: A 12-month study. J Indian Soc Periodontol 2013. [Google Scholar]
- Z Menceva, O Dimitrovski, M Popovska, S Spasovski, V Spirov, G Petrusevska. Free gingival graft versus mucograft: histological evaluation. Open Access Maced J Med Sci 2018. [Google Scholar]
- M Sanz, R Lorenzo, J J Aranda, C Martin, M Orsini. Clinical evaluation of a newcollagen matrix(Mucograft®prototype) to enhance the width of keratinized tissue in patients with fixed prosthetic restorations: a randomized prospective clinical trial. J Clin Periodontol 2009. [Google Scholar]
- P D Miller. A classification of marginal tissue recession. Int J Periodontics Restor Dent 1985. [Google Scholar]
- A Vrushali, W David, M Jules. Treatment of a mandibular anterior lingual recession defect with minimally invasive laterally closed tunneling technique and sub-epithelial connective tissue graft. Int Arch Maxillofac Surg 2018. [Google Scholar]
- A Moreira, M P Santamaria, K G Silvério. Coronally advanced flap with or without porcine collagen matrix for root coverage: a randomized clinical trial. Clin Oral Investig 2016. [Google Scholar]
- R Rotundo, G Pini-Prato. Use of a new collagen matrix (mucograft) for the treatment of multiple gingival recessions: case reports. Int J Periodontics Restor Dent 2012. [Google Scholar]
